A manual work crossword is an engaging educational tool that combines problem-solving with learning about various occupations and tools. It offers an interactive way to explore manual labor through clues and answers, making it both fun and informative for learners of all ages.
By focusing on themes like jobs, tools, and workplace terminology, these crosswords enhance vocabulary, critical thinking, and knowledge about manual work, providing a unique learning experience that appeals to both students and enthusiasts alike.
1.1. Definition of Manual Work
Manual work refers to tasks that require physical skill and effort, often involving tools or machinery. It encompasses a wide range of activities, from construction and manufacturing to farming and craftsmanship. In the context of crossword puzzles, manual work clues often highlight occupations, tools, and techniques, offering a fun way to learn about various trades and industries. These clues not only test knowledge but also encourage problem-solving and critical thinking, making them engaging for learners of all levels.
1.2. Importance of Crossword Puzzles in Learning
Crossword puzzles are a valuable educational tool that enhances cognitive skills, vocabulary, and problem-solving abilities. They engage learners by combining fun with mental challenges, making complex topics more accessible. For manual work crosswords, they provide an interactive way to explore occupations, tools, and techniques, fostering a deeper understanding of manual labor. Crosswords cater to diverse learning styles and encourage critical thinking, making them a versatile resource for both entertainment and education.
1.3. Relevance of Manual Work in Crossword Clues
Manual work serves as a rich theme for crossword clues, offering diverse content related to jobs, tools, and workplace terminology. Clues often reference occupations such as scientists, actors, pilots, chefs, and miners, making crosswords an engaging way to explore various professions. Additionally, tools and machinery commonly associated with manual labor are frequent elements in crossword puzzles, enhancing problem-solving skills while educating participants about different trades and industries. This thematic focus ensures that crosswords remain both entertaining and educational.
Types of Manual Work
Manual work encompasses various industries, including construction, manufacturing, farming, and craftsmanship. Each type involves hands-on tasks, requiring specific skills and tools, making them diverse and essential.
2.1. Construction Work
Construction work involves building, repairing, and maintaining infrastructure. It requires physical labor and technical skills, often using tools like hammers, drills, and cranes. Workers may face challenges like heavy workloads and safety risks. Crossword clues related to construction might include terms like “hammer,” “scaffold,” or “cement,” testing solvers’ knowledge of the trade. This sector is vital for developing communities and provides a sense of accomplishment for those involved.
Engaging with construction-themed crosswords can enhance understanding of the industry while offering an enjoyable puzzle-solving experience for enthusiasts and professionals alike.
2.2. Manufacturing Jobs
Manufacturing jobs involve the production of goods using machinery and tools. These roles often require precision, attention to detail, and physical stamina. Workers may operate equipment, assemble parts, or quality-check products. Crossword clues might include terms like “assembly line,” “welder,” or “blueprint.” Manufacturing is crucial for economic growth and innovation, offering a sense of pride in creating tangible products. Solving manufacturing-themed crosswords can help learners familiarize themselves with industry-specific terminology and concepts while enjoying a challenging puzzle.
Engaging with these crosswords fosters a deeper appreciation for the skills and processes behind modern manufacturing.
2.3. Farming and Agricultural Work
Farming and agricultural work involve cultivating land, growing crops, and raising livestock. These jobs require physical endurance, practical skills, and a deep connection to nature. Crossword clues might include terms like “plow,” “harvest,” or “tractor.” Agricultural workers play a vital role in food production, ensuring communities have access to fresh produce and animal products. Engaging with farming-themed crosswords can educate participants about the tools, techniques, and challenges faced in this essential field, while also celebrating the hard work behind our daily sustenance.
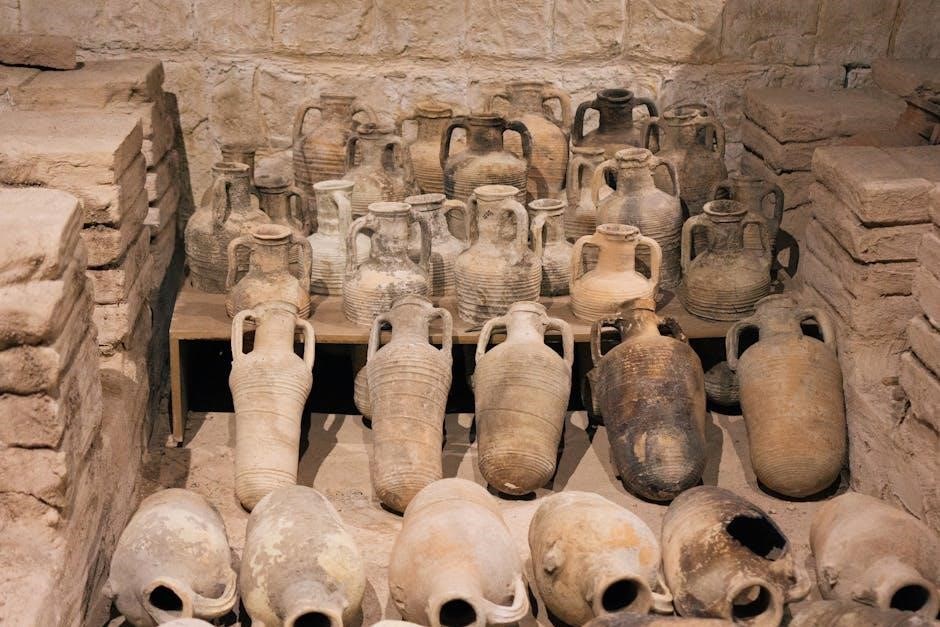
2.4. Craftsmanship and Artisanal Work
Craftsmanship and artisanal work involve creating items with skill and precision, often by hand. These trades require dedication, creativity, and mastery of techniques passed through generations. From woodworking to pottery, artisans produce unique, high-quality products that reflect their expertise. In crosswords, clues related to craftsmanship might include terms like “chisel,” “loom,” or “k Kiln.” These puzzles celebrate the artistry and effort behind handmade goods, offering a fun way to explore the world of craftsmanship while testing your knowledge of tools, materials, and traditional practices.

Tools and Equipment in Manual Work
Manual work relies on tools and equipment to enhance efficiency and accuracy. From hand tools like hammers to power tools like drills, and safety gear, these items are essential for tasks and often appear in crossword clues, aiding puzzle solvers in understanding manual labor processes.
3.1. Hand Tools
Hand tools are essential for manual work, offering precision and control. Common examples include hammers, screwdrivers, pliers, and wrenches. These tools are often featured in crossword clues, with their names frequently appearing as answers. They require skill and are integral to various trades, making them a staple in crossword puzzles related to manual labor; Solvers often recognize these terms, aiding in problem-solving. Their versatility and ubiquity in manual tasks make them a key focus in crossword clues tied to hand tools and equipment.
3.2. Power Tools
Power tools are electric or battery-operated devices that enhance efficiency in manual tasks. Examples include drills, saws, sanders, and impact wrenches. These tools are widely used in construction, woodworking, and metalworking. In crossword puzzles, terms like “drill” or “sander” often appear as clues or answers. Solving such clues requires familiarity with tool terminology and their applications. Power tools are indispensable in modern manual work, making them a common theme in crossword puzzles related to trades and craftsmanship. Their versatility and prevalence ensure they remain relevant in both work and puzzle contexts.
3.3. Safety Equipment
Safety equipment is crucial for protecting workers in manual tasks. Items like helmets, gloves, safety glasses, and harnesses are commonly used to prevent injuries. In crossword puzzles, terms such as “hard hat” or “PPE” (Personal Protective Equipment) often appear as clues or answers. These clues highlight the importance of safety in manual labor. Understanding safety equipment terminology can help solvers complete crosswords accurately. Safety gear is essential in various industries, making it a frequent theme in puzzles related to manual work and workplace safety protocols.

Safety and Health in Manual Work
Safety and health are vital in manual work, involving hazard identification, injury prevention, and promoting worker well-being. Proper practices and training reduce risks, ensuring a safer environment.
4.1. Workplace Safety Measures
Workplace safety measures are essential to prevent accidents and ensure a secure environment for manual labor. These include conducting regular risk assessments, implementing safety protocols, and providing personal protective equipment (PPE). Training employees on proper techniques and emergency procedures is crucial. Maintaining clean and organized workspaces reduces hazards. Employers must enforce safety standards and encourage a culture of safety awareness. Regular inspections and updates to safety policies help adapt to changing work conditions, ensuring the well-being of all workers engaged in manual tasks. Adherence to these measures minimizes risks and fosters a safer workplace.
4.2. Common Injuries in Manual Labor
Manual labor often leads to injuries due to physical strain and repetitive tasks. Musculoskeletal disorders, such as back pain and joint issues, are prevalent. Cuts, abrasions, and bruises result from handling sharp tools or heavy materials. Strains and sprains occur from lifting or overexertion. Repetitive stress injuries, like carpal tunnel syndrome, are common in tasks requiring constant motion. Fractures and head injuries can occur from falls or falling objects. These injuries highlight the need for proper training and precautions to ensure worker safety and reduce long-term health impacts in manual work environments.
4.3. Ergonomics in Manual Tasks
Ergonomics focuses on optimizing manual tasks to minimize physical strain and enhance efficiency. Proper posture, tool design, and workspace layout are key to reducing discomfort. Implementing ergonomic practices can lower the risk of musculoskeletal injuries and fatigue. Techniques include alternating tasks, using assistive devices, and ensuring adequate rest periods. Training workers in ergonomic principles improves safety and productivity, creating a healthier work environment. By aligning tasks with human capabilities, ergonomics promotes long-term well-being and job satisfaction in manual labor roles.

Benefits of Manual Work
Manual work enhances physical fitness, boosts mental clarity, and fosters a sense of accomplishment, contributing to overall well-being and personal growth through hands-on engagement and skill mastery.
5.1. Physical Health Benefits
Manual work improves cardiovascular health, strengthens muscles, and enhances flexibility through consistent physical activity. It reduces obesity risks and boosts endurance, making it a holistic way to stay fit. Regular engagement in manual tasks promotes better posture and balance, while also improving hand-eye coordination. These physical benefits contribute to overall longevity and energy levels, making manual work a valuable practice for maintaining a healthy lifestyle. Such themes often appear in crossword clues, highlighting terms like “strength” or “endurance.”
5.2. Mental and Emotional Well-being
Manual work fosters mental clarity and reduces stress by providing a sense of accomplishment. Engaging in hands-on tasks enhances problem-solving skills and creativity. It also promotes mindfulness, as focus is directed toward the task at hand. The satisfaction from creating or repairing something boosts self-esteem and confidence. Additionally, manual labor can delay cognitive decline and improve overall emotional resilience. These mental benefits often inspire crossword clues related to terms like “stress relief” or “confidence,” linking manual work to emotional well-being.
5.3. Skill Development and Pride in Work
Manual work enhances skill development by refining dexterity, precision, and problem-solving abilities. Mastery of tasks builds confidence and fosters a sense of accomplishment. Pride in work is deeply rooted in creating something tangible, whether crafting furniture or repairing machinery. This satisfaction often translates into crossword clues like “craftsmanship” or “expertise,” celebrating the value of skilled labor. The process of learning and perfecting trades encourages resilience and self-reliance, making it a rewarding aspect of manual work.

Training and Education for Manual Work
Manual work training involves structured programs that combine theoretical knowledge with hands-on experience, equipping individuals with practical skills for various trades and ensuring workplace readiness.
6.1. Vocational Training Programs
Vocational training programs, often referred to as trade schools, focus on equipping individuals with specific skills for manual work. These programs emphasize hands-on experience, preparing students for careers in trades like plumbing, electrical work, or carpentry. Typically shorter than traditional degree programs, they offer practical knowledge through workshops, apprenticeships, and real-world applications. Vocational training is designed to ensure job readiness, making it an essential pathway for those pursuing manual labor careers. The emphasis on manual skills aligns perfectly with crossword clues related to trades and tools.
6.2. Apprenticeships
Apprenticeships are structured training programs combining on-the-job experience with theoretical instruction. They allow individuals to learn manual work skills under experienced professionals. Typically lasting several years, apprenticeships cover trades like welding, machining, or electrical work. Participants earn wages while gaining practical expertise, often leading to certifications. This hands-on approach ensures mastery of tools and techniques, making apprenticeships invaluable for manual labor careers. The real-world application of skills aligns closely with crossword clues involving trades, tools, and workplace terminology, enhancing problem-solving abilities for related puzzles;
6.3. Certification Courses
Certification courses provide specialized training for manual work, offering in-depth knowledge of specific trades or skills. These short-term programs are often designed for individuals seeking to enhance their expertise in areas like machinery operation, safety protocols, or tool usage. Examples include OSHA certifications for workplace safety or equipment-specific training. These courses are valuable for both career advancement and improving problem-solving skills, as they familiarize participants with industry terminology and concepts often found in crossword clues related to manual labor and workplace environments.

Industry Trends in Manual Work
The manual work industry is evolving with automation, green jobs, and globalization. These trends enhance efficiency, sustainability, and global connectivity, reshaping traditional labor practices.
7.1. Automation and Technology Integration
Automation and technology are revolutionizing manual work, enhancing efficiency and precision. Robotics, AI, and smart tools reduce physical strain, improve safety, and streamline repetitive tasks. These advancements enable workers to focus on complex problem-solving, fostering innovation. However, they also require upskilling to adapt to new systems. Crossword clues might relate to terms like “robotics” or “AI tools,” reflecting this modern shift in manual labor practices.
7.2. Green Jobs and Sustainability
Green jobs and sustainability are transforming manual work, emphasizing eco-friendly practices. Roles like solar panel installers and recycling specialists are gaining prominence. Crossword clues might include terms like “renewable energy” or “sustainable materials.” These jobs align with global efforts to reduce environmental impact, blending traditional manual skills with modern eco-conscious approaches. Such positions highlight the evolving nature of manual labor, where sustainability is both a challenge and an opportunity for innovation and growth in the workforce.
7.3. Globalization of Manual Labor
Globalization has significantly impacted manual labor, creating a interconnected workforce across borders. Industries like construction, manufacturing, and agriculture now rely on international labor markets. Crossword clues might reference terms like “outsourcing” or “offshoring,” reflecting how manual jobs are distributed worldwide. This trend has reshaped economies, influencing wages, cultural exchange, and job availability. While it offers opportunities, it also poses challenges like competition and ethical concerns, making it a complex yet vital aspect of modern manual work.

Cultural Significance of Manual Work
Manual work embodies societal values, craftsmanship, and creativity, often celebrated in art, literature, and traditions, fostering community identity and pride in tangible contributions.
8.1. Historical Perspectives
Manual work has deep historical roots, with ancient civilizations relying on it for survival and progress. From constructing monumental structures like the Pyramids to crafting tools, manual labor shaped societies. Historical records highlight the respect for skilled workers, such as blacksmiths and carpenters, who were vital to community development. The Middle Ages saw the rise of guilds, formalizing craftsmanship and setting standards. Even today, historical practices influence modern manual work, preserving traditions while adapting to new technologies. Crossword clues often reflect this rich history, connecting players to the past.
8.2. Regional Variations in Manual Labor
Manual labor varies significantly across regions due to cultural, environmental, and economic factors. In Asia, rice cultivation and tea plantations dominate, while Africa focuses on artisanal crafts and subsistence farming. Europe emphasizes precision craftsmanship, with countries like Germany and Italy renowned for skilled trades. The Americas blend indigenous techniques with modern agriculture and construction. These regional differences are reflected in crossword clues, often requiring knowledge of local tools, practices, and terminology. Solving such clues offers insight into global work traditions and cultural diversity.
8.3. Art and Literature Depicting Manual Work
Manual work has been a recurring theme in art and literature, reflecting its cultural and historical significance. Paintings like The Gleaners by Jean-François Millet highlight agricultural labor, while authors like John Steinbeck portray the lives of workers in novels such as The Grapes of Wrath. These depictions often inspire crossword clues, with references to tools, trades, or literary characters. Such connections enrich puzzles, offering solvers a glimpse into the artistic and literary celebration of manual labor and its enduring impact on human society.

Common Crossword Clues Related to Manual Work
Manual work crosswords often feature clues about tools, trades, and tasks, challenging solvers to connect hands-on labor with wordplay, making puzzles engaging and educational.
9.1. Occupations
Manual work crosswords often include clues related to various occupations, such as carpenter, electrician, plumber, or mechanic. These professions require hands-on skills and are frequently referenced in puzzles. Other common clues might involve laborers, construction workers, or farmers, highlighting roles that emphasize physical effort. Additionally, terms like “tradesperson” or “craftsman” often appear, testing solvers’ knowledge of job titles. These clues not only challenge but also educate players about different manual trades and their significance in society, making the crossword both entertaining and informative.
9.2. Tools and Machinery
Manual work crosswords frequently include clues about tools and machinery, such as wrenches, hammers, or drills. These terms are often used in puzzles, testing solvers’ familiarity with equipment used in various trades. Clues might range from specific power tools like “circular saw” to broader categories like “hand tool.” Additionally, machinery like forklifts or cranes might appear, adding diversity to the clues. These references not only challenge players but also highlight the essential role of tools in manual labor, making crosswords both entertaining and educational.
9.3. Workplace Terminology
Workplace terminology often appears in manual work crosswords, testing solvers’ knowledge of industry-specific language. Terms like “workshop,” “shift,” or “safety” are common clues. Other examples include “apprentice,” “foreman,” or “blueprint.” These words reflect the daily operations and roles within manual labor environments. Clues might also involve slang or jargon, such as “toolkit” or “hard hat.” Understanding these terms enhances problem-solving skills and familiarity with workplace culture, making crosswords a fun way to learn about manual work environments and their unique vocabulary.

Solving Manual Work Crossword Clues
Solving manual work crosswords requires understanding industry-specific terms and applying logical thinking. Start with easy clues, then build momentum by connecting related words. Practice improves skill and speed, making the process enjoyable and rewarding for enthusiasts of manual labor themes.
10.1. Tips for Beginners
Start by focusing on shorter clues, as they often provide clearer answers. Look for common industry terms related to manual work, such as tools or professions. Use word overlaps strategically to connect clues. Eliminate incorrect options by crossing out letters you know aren’t right. Don’t hesitate to guess—many crossword clues rely on context. Practice regularly to build familiarity with manual work terminology and improve your problem-solving skills. Patience and persistence are key to mastering these puzzles.
10.2. Advanced Strategies
For experienced solvers, advanced techniques involve analyzing clue patterns and recognizing common word roots. Focus on clues related to tools or machinery, as these often repeat in manual work themes. Cross-reference answers by identifying shared letters in adjacent clues. Use word roots and common suffixes or prefixes to deduce answers more efficiently. Expand your vocabulary with industry-specific terms using resources like thesauruses or trade glossaries. Learn from mistakes to refine your approach and maintain a crossword journal to track progress and note frequently used terms.
10.3. Common Pitfalls to Avoid
When solving manual work crosswords, avoid rushing through clues without understanding context. Misinterpreting clues as too literal or overcomplicating them is common. Don’t overlook wordplay like anagrams or homonyms. Guessing without evidence can lead to errors, so focus on eliminating impossible answers first. Overreliance on familiar terms may distract from less obvious solutions. Keep track of letters already used to avoid repetition. Practice patience and methodical thinking to enhance accuracy and enjoyment of the puzzle.
The manual work crossword concludes the journey through its significance, celebrating the importance of labor while enhancing knowledge and sharpening problem-solving skills, fostering appreciation for skilled trades.
11.1. Summary of Key Points
Manual work is essential for various industries, requiring skill and dedication. Crosswords highlight its importance by incorporating related terms, fostering learning through interactive puzzles. The exploration of types of manual work, tools, and safety measures underscores its complexity. Benefits like physical health and mental well-being, along with skill development, emphasize its value. Training programs and industry trends further illustrate its evolution. Crosswords make learning engaging, encouraging appreciation for the craftsmanship and labor that shape our world, while promoting problem-solving and knowledge retention in an enjoyable way.
11.2. Encouragement for Further Learning
Engaging with manual work crosswords fosters a deeper appreciation for hands-on skills and problem-solving. Exploring more puzzles and resources can enhance your knowledge of tools, trades, and workplace terminology. Connecting with communities or experts in manual labor can further enrich your understanding. Continuous learning through crosswords and real-world applications encourages personal growth and intellectual curiosity. Embrace the challenge and enjoy the journey of mastering manual work crosswords while expanding your skill set and appreciation for the craftsmanship behind everyday tasks.
11.3. Final Thoughts on Manual Work Crossword
Manual work crosswords offer a unique blend of entertainment and education, making them an excellent tool for learners. By solving clues related to tools, trades, and techniques, participants gain a deeper understanding of manual labor’s significance. This engaging activity not only sharpens cognitive skills but also fosters an appreciation for the craftsmanship behind everyday tasks. Embrace the challenge, enjoy the process, and continue exploring the fascinating world of manual work through crosswords. It’s a rewarding journey that combines fun with knowledge!